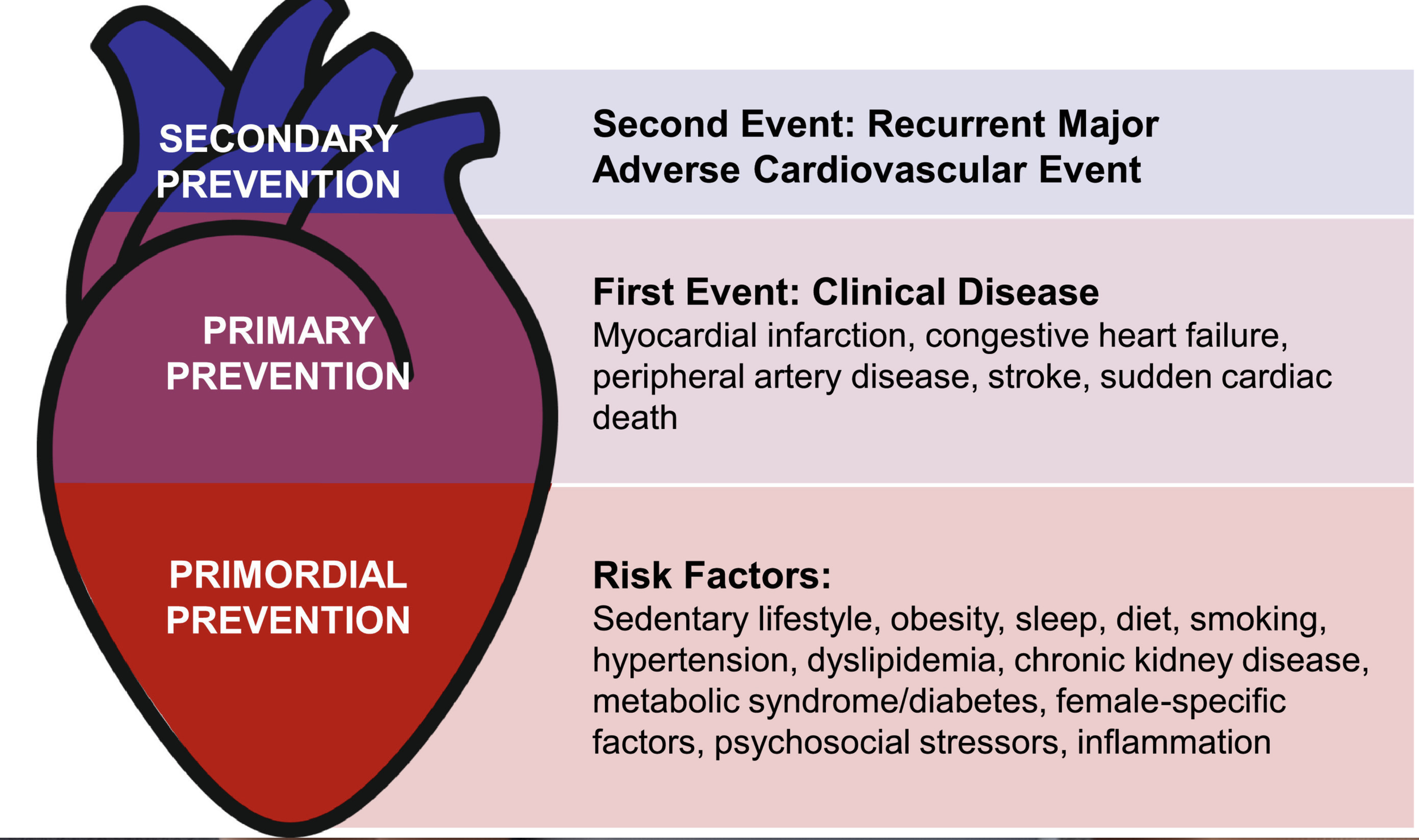
Preventive cardiology is a subspecialty of cardiovascular medicine focused on lowering the risk of developing heart disease and its complications (heart attack, stroke, heart failure) in individuals who have not yet experienced a major cardiovascular event.
It emphasizes early detection, risk factor modification, and evidence-based interventions before clinical disease becomes manifest.
Preventive Cardiology
The ultimate goal is to prevent the first heart attack or stroke rather than treating disease after it occurs.
Key Features:
-
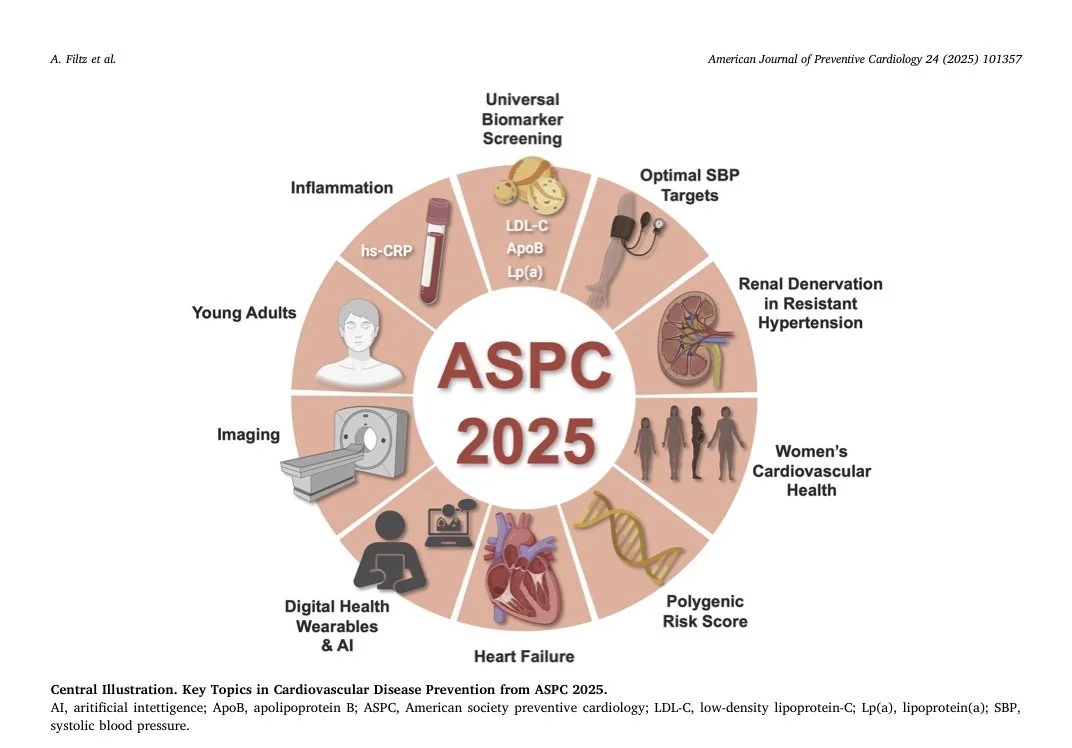
Incorporating Emerging and Enhancing Risk Factors for Appropriate and Prompt Risk Stratification and Management
Screen all childbearing-age women with CVD using mWHO 2.0, incorporating biomarkers/genetics/social factors.
Preconception Counseling: Optimize health (e.g., BP, weight), switch contraindicated meds, and discuss contraception. Genetic testing and risk tool application guide decisions
During Pregnancy: Serial monitoring (TTE in high-risk, biomarkers), lifestyle interventions (Mediterranean diet, exercise), and prophylaxis (LMWH for VTE, aspirin for PE). Address acute events
Assemble PHT for high-risk patients; optimize preconception and monitor dynamically
Social Determinants and Environmental Factors: Ethnicity (e.g., higher VTE mortality in Black women), socioeconomic status, obesity (BMI ≥35), age , and geography (e.g., higher PPCM in certain regions) amplify risks. Addressing disparities through remote monitoring
Follow-up postpartum for 3-6-12 months, addressing long-term CV risk from APOs
-
Using CT scans to detect subclinical atherosclerosis and guide intensity of therapy (in select patients if needed)
-
Diabetes is a growing epidemic in the United States, affecting approximately 38 million people (about 11-12% of the population), with around 1 in 5 cases undiagnosed. Recent data (2021–2023) show total prevalence among adults at roughly 14.3% (including undiagnosed), higher in men and linked to obesity and aging. An additional 98 million adults have prediabetes, underscoring the ongoing public health crisis.
At ACC we focus on comprehensive cardiovascular risk reduction while collaborating with primary care, endocrinology, and multidisciplinary teams, playing a pivotal role in bridging glucocentric and cardiorenal-metabolic care
Aggressively manage modifiable risk factors — Target blood pressure <130/80 mmHg , optimize lipids with high-intensity statins (and PCSK9 inhibitors if needed), promote smoking cessation, and ensure antiplatelet therapy where indicated.
Prioritize cardio-protective glucose-lowering therapies — GLP-1 receptor agonists (e.g., semaglutide) and/or SGLT2 inhibitors (e.g., empagliflozin)
Emphasize lifestyle interventions — Counsel on weight loss (≥5-10%), Mediterranean or plant-based diets low in saturated fats, ≥150 minutes/week moderate aerobic activity, and sleep optimization—these are foundational for preventing progression from prediabetes and reducing CV events.
Screen and prevent early — Identify prediabetes in at-risk patients (e.g., obesity, family history); (lifestyle-based, proven to reduce incidence by ~58% in high-risk groups) or consider metformin for prevention in select cases
Adopt a multidisciplinary, patient-centered approach — Coordinate care to address social determinants, ensure medication adherence, and monitor for complications like silent ischemia
-
Genetic dyslipidemias, particularly familial hypercholesterolemia (FH), represent a significant yet underdiagnosed cause of premature atherosclerotic cardiovascular disease (ASCVD).
We offer:
Screen high-risk patients (e.g., premature ASCVD history) with advanced lipid panels including ApoB and Lp(a), alongside genetic evaluation for FH.
If FH is suspected or confirmed, initiate cascade screening and high-intensity lipid-lowering therapies
Shared decision-making to discuss genetic counseling, lifestyle modifications, and novel agents.
Monitor periodically and adjust based on response, integrating with comprehensive CV risk management
-
Early and intensive blood pressure lowering to prevent heart attacks, heart failure, kidney failure, blindness, loss of memory, and other issues
-
Chronic low-grade inflammation plays a central role in the pathogenesis of atherosclerosis and cardiovascular disease (CVD). Even with optimal control of traditional risk factors (e.g., LDL cholesterol, blood pressure, diabetes), many patients exhibit residual inflammatory risk—persistent systemic inflammation that drives recurrent events.
High-sensitivity C-reactive protein (hs-CRP) is the most validated, inexpensive, and widely available biomarker for assessing this risk.
In patients with established CVD (secondary prevention), hs-CRP levels are at least as predictive of recurrent events as LDL cholesterol, even on statin therapy (per 2025 ACC Scientific Statement on Inflammation and CVD)
Broad screening is recommended for most secondary prevention patients to identify residual inflammatory risk (2025 ACC Statement).
In primary prevention, hs-CRP serves as a risk enhancer in intermediate-risk individuals (per 2018/2019 AHA/ACC guidelines).
We offer:
Screen primary & secondary prevention in select patients with hs-CRP alongside lipids
If hs-CRP is elevated despite optimal GDMT, reinforce lifestyle interventions (e.g., ≥150 min/week exercise, Mediterranean/DASH diet, omega-3 intake, smoking cessation) and consider adding low-dose colchicine after shared decision-making
-
Medically supervised programs combining exercise prescription, nutrition counseling, and smoking cessation
-
We go beyond the traditional lipid panel.
Based on individualized risk profile, we assess Lp(a), ApoB, hsCRP (cardiac specific)
Aggressive treatment of high LDL cholesterol with effective therapies: statins, PCSK9 inhibitors, or newer agents in high-risk patients
-
Microvascular angina (MVA), also known as coronary microvascular dysfunction (CMD) or angina with no obstructive coronary arteries (ANOCA), is a form of stable angina caused by abnormalities in the small coronary arteries (microvasculature) rather than blockages in the major epicardial vessels. Affecting up to 50% of patients undergoing angiography for chest pain, MVA is more common in women, postmenopausal individuals, and those with cardiometabolic risk factors like diabetes, hypertension, or obesity. It leads to ischemia, reduced quality of life, and increased risk of major adverse cardiovascular events (MACE), despite normal-appearing coronaries on standard angiography. Early diagnosis through dedicated cath lab testing is crucial, as it enables targeted management to alleviate symptoms and improve outcomes
Screen patients with angina and normal coronaries using noninvasive tools (e.g., PET/CT for CFR).
Dedicated cath lab testing to confirm MVA and classify endotype.
Tailor management with shared decision-making, starting with lifestyle and escalating pharmacotherapy.
Reassess at 3-6 months; coordinate multidisciplinary care for optimal outcomes.